Periodontal disease is one of the most common threats to long-term oral health, yet it often progresses quietly. One of its key warning signs is the development of periodontal pockets—spaces that form between the teeth and gums when infection damages the supporting tissues. In a healthy mouth, the gums are closely attached to the teeth, and the gingival margin forms a tight seal around each tooth, helping to protect against bacteria and prevent the formation of periodontal pockets. A common question patients ask is whether these pockets can be reversed, but the answer depends on the severity of the condition and how early treatment begins.
This article explains what is a periodontal pocket, why periodontal pockets matter for gum health, how they are diagnosed, and the treatment options available to help stop disease progression and restore a healthy mouth.
What Is a Periodontal Pocket?
To understand whether healing is possible, it helps to first clarify what is a periodontal pocket. A periodontal pocket is a deepened, diseased gap between the tooth and surrounding gum tissue. In healthy gums, the gingival margin forms a tight seal at the gum line, and this space measures between 1 and 3 millimeters and fits snugly around the tooth. A healthy gum sulcus is anywhere up to 3mm deep.
When bacterial plaque and tartar build up along and below the gumline, they trigger inflammation that causes the gums to detach from the tooth. As the gum pulls away, the space deepens and becomes a periodontal pocket. These pockets trap bacteria, making them difficult to clean with routine brushing and flossing and allowing the disease to progress further.
Why Periodontal Pockets Are Dangerous for Gum Health
Periodontal pockets play a central role in the progression of gum disease. Once pockets deepen beyond healthy limits, they create an environment where harmful bacteria thrive. Over time, this infection can destroy gum tissue and the underlying bone that supports the teeth. Periodontal pockets can capture and hold bacteria, especially plaque bacteria, which can cause damage to the jaw bone where teeth are anchored.
Untreated periodontal pockets can lead to:
- Chronic gum infection
- Progressive bone loss
- Gum recession
- Tooth mobility or shifting
- Eventual tooth loss, as teeth can loosen and eventually fall out if left untreated.
Bacteria from periodontal pockets can enter the bloodstream, increasing the risk of heart disease, diabetes complications, and stroke. Active gum disease also increases the risk and severity of these systemic health conditions.
Because the damage often occurs below the gumline, many patients are unaware of the problem until it becomes advanced.
What Do Periodontal Pockets Look Like?
Although periodontal pockets themselves are not visible to the naked eye, they often cause noticeable symptoms in the gums and teeth.
Visible symptoms may include:
- Bright red, swollen gums, or purplish gums
- Gums that feel tender or bleed easily
- Receding gumline, making teeth appear longer
- Spaces developing between teeth
- Loose or shifting teeth
Gum pockets are often associated with these symptoms. Signs of periodontal pockets may include gums that bleed during brushing, persistent bad breath, visible pus around the gumline, and pain when chewing.
Common Visible Symptoms
- Bright red, swollen, or purplish gums
- Gums that bleed easily when brushing or flossing
- Gum recession that makes teeth appear longer
- Persistent bad breath or a bad taste in the mouth
- Teeth that feel loose or have shifted position

Measuring Periodontal Pocket Depth
Dentists and periodontists measure periodontal pockets using a periodontal probe. The depth is recorded in millimeters:
- 1–3 mm: Healthy, normal gum attachment
- 4 mm: Borderline pocket depth that requires monitoring
- 5–6 mm: Moderate periodontal disease
- 7+ mm: Severe periodontal disease with significant tissue and bone loss
These measurements guide treatment planning and help determine whether periodontal pockets can be reduced.

Causes and Risk Factors of Periodontal Pockets
Several factors contribute to the formation of periodontal pockets, including:
- Plaque and Tartar Buildup: Bacteria in plaque cause inflammation that separates the gum from the tooth
- Poor Oral Hygiene: Inadequate brushing and flossing allow plaque to harden into tartar
- Smoking or Tobacco Use: A major risk factor that impairs healing
- Genetics: Some individuals are more susceptible to gum disease
- Health Conditions: Diabetes, stress, and hormonal changes can increase risk
Regular dental cleanings and good oral hygiene help remove plaque and are essential to prevent periodontal disease. Early detection is important to catch gum disease before it progresses and causes more severe damage.
Identifying and managing these factors is essential for successful treatment.
Can Periodontal Pockets Be Reversed?
The reversibility of periodontal pockets depends on their depth and the extent of tissue and bone damage.
- Early-stage or mild periodontal pockets can often be reduced and stabilized with non-surgical treatment and improved oral hygiene.
- Moderate to severe periodontal pockets may not be fully reversible, but their depth can often be reduced and the disease controlled with advanced therapies.
The primary goal of treatment is to remove bacteria, stop further destruction, and encourage the gums to reattach to the tooth as much as possible.
Treatment of periodontal pockets focuses on removing bacteria and reducing pocket depth, which may include scaling and root planing or surgery. These steps help prevent periodontal pockets from worsening or recurring.
Non-Surgical Treatments for Periodontal Pockets
For mild to moderate cases, non-surgical therapies are often effective in reducing periodontal pocket depth.
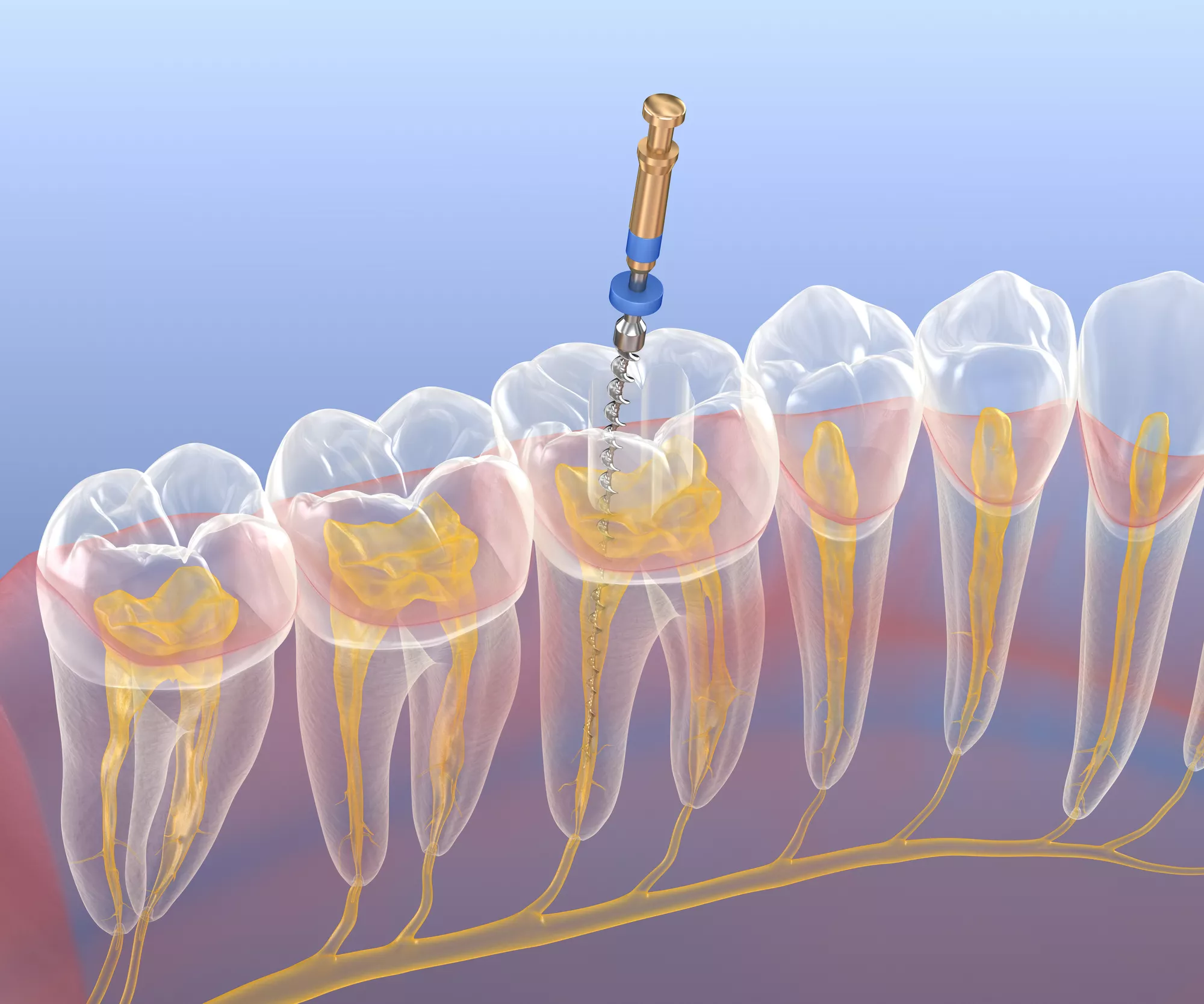
Scaling and Root Planing
Scaling and root planing is a non-surgical dental procedure that helps remove bacteria, plaque, and tartar from around teeth. An ultrasonic device is often used during scaling and root planing to remove deposits and smooth the root surfaces. The tooth root surfaces are smoothed to discourage future bacterial buildup and allow the gums to reattach more securely.
Perioscopy
Perioscopy, also known as dental endoscopy, is a minimally invasive approach to treating periodontal pockets in certain cases. Using a tiny camera inserted below the gumline, this technology allows clinicians to clearly visualize plaque, tartar, and infected root surfaces with magnification. This enhanced visibility enables more precise and thorough cleaning of the periodontal pocket and may help some patients avoid traditional gum surgery.
Antibiotic Therapy
Topical gels, oral antibiotics, or prescription antimicrobial rinses such as chlorhexidine may be used to reduce bacterial infection within the periodontal pocket. Localized antibiotics may be placed in the pockets of periodontal disease to kill bacteria, and antibacterial gels can be applied directly into periodontal pockets after scaling and root planing to reduce inflammation. Antibacterial mouthwash can also be recommended as part of an at-home oral hygiene routine to help control bacteria.
Professional Periodontal Maintenance
Patients with periodontal disease often require more frequent cleanings—typically every three to four months—to maintain results and prevent recurrence.
Enhanced Home Care
Improved daily oral hygiene is critical. This may include meticulous brushing, flossing, and the use of a water flosser with a specialized tip designed to clean deep periodontal pockets.

Surgical Treatments for Severe Periodontal Pockets
When periodontal pockets are deep or accompanied by bone loss, surgical intervention may be necessary. Surgical treatments aim to restore gum and bone health around your teeth.
Pocket Reduction (Flap) Surgery
In this procedure, the gums are gently lifted back so that deep tartar deposits can be thoroughly removed. The gum tissue is then repositioned to reduce pocket depth and make the area easier to keep clean.
Regenerative Procedures
When bone or connective tissue has been lost, bone grafting is a procedure where bone grafting material is placed into areas where bone has eroded due to gum disease. Bone grafts or regenerative membranes may be used to encourage the body to rebuild lost support structures around the teeth.
Gum grafting, also known as soft tissue grafts, is used to add tissue to areas of gum recession and cover exposed tooth roots. Guided tissue regeneration is another surgical option that promotes the regrowth of lost bone and supporting tissues around the teeth, especially in cases with deep periodontal pockets and bone loss.
Laser Therapy (LANAP)
Laser-assisted periodontal therapy uses a precise, minimally invasive laser to remove diseased tissue and bacteria while promoting healing and potential bone regeneration.
The choice of treatment depends on pocket depth, bone loss, overall health, and individual patient needs.
Periodontal Care at Foundation Dental Specialists in Pasadena
At Foundation Dental Specialists in Pasadena, our team of experienced periodontists and endodontists is passionate about providing advanced, patient-centered periodontal care. We understand that every case of periodontal pockets is unique, which is why we offer a wide range of dental services to treat complex gum and tooth conditions.
By creating customized treatment plans based on strong scientific evidence, clinical judgment, experience, and patient preference, our specialists are able to deliver highly successful oral health solutions. Our goal is not only to treat periodontal disease, but to lay the foundation for confident, healthy smiles that last.

Take the Next Step Toward Healthier Gums. Contact Foundation Dental Specialist Today
If you are experiencing symptoms of gum disease or have been told you have periodontal pockets, early treatment can make a significant difference. Whether periodontal pockets can be reversed or simply managed, professional care is essential to protecting your oral health.
Contact Foundation Dental Specialists today to schedule a consultation or appointment. Our team is here to help you restore your gum health and build a strong foundation for a healthier smile.
Frequently Asked Questions
What is a periodontal pocket?
A periodontal pocket is a diseased space that forms between the tooth and gum when plaque and bacteria cause the gum tissue to pull away. These pockets allow bacteria to collect below the gumline, increasing the risk of infection, bone loss, and tooth loss.
Can periodontal pockets be reversed?
Mild periodontal pockets can often be reduced or stabilized with early treatment and excellent oral hygiene. Deeper periodontal pockets may not be fully reversible, but professional care can significantly reduce their depth and prevent further damage.
What causes periodontal pockets to form?
Periodontal pockets are primarily caused by the accumulation of plaque bacteria and tartar buildup, which lead to gum inflammation and infection. Risk factors such as poor oral hygiene, smoking, genetics, diabetes, and stress can accelerate their development.
What do periodontal pockets look like?
While periodontal pockets themselves are not visible, they often cause red, swollen, bleeding, or receding gums. Other signs may include bad breath, tooth sensitivity, or teeth that appear longer due to gum recession.
Are periodontal pockets painful?
Periodontal pockets are often painless in the early stages, which is why gum disease can go unnoticed. As the condition progresses, patients may experience tenderness, swelling, bleeding, or discomfort when chewing.
What treatments are available for periodontal pockets?
Treatment options range from non-surgical deep cleanings like scaling and root planing to surgical procedures such as pocket reduction surgery, regenerative therapy, or laser treatment. The best approach depends on pocket depth and the amount of bone loss.
What happens if periodontal pockets are left untreated?
Untreated periodontal pockets can lead to chronic infection, progressive bone loss, loose teeth, and eventual tooth loss. Gum disease has also been linked to systemic health issues, making early treatment especially important.
Do periodontal pockets always require surgery?
No, many periodontal pockets can be treated successfully with non-surgical methods when caught early. Surgery is typically recommended only for deep pockets that do not respond to conservative treatment.
Can periodontal pockets come back after treatment?
Yes, periodontal pockets can recur if plaque control is poor or maintenance visits are skipped. Ongoing professional cleanings and consistent home care are essential for long-term gum health.
How often should I see a dentist if I have periodontal pockets?
Patients with periodontal disease often need professional cleanings every three to four months. These visits help control bacteria and monitor pocket depth to prevent recurrence.
When should I see a periodontist for periodontal pockets?
You should see a periodontist if your dentist detects deep periodontal pockets, gum recession, or bone loss. Periodontists specialize in treating advanced gum disease and preserving natural teeth whenever possible.